Evolving landscape of lymphoma treatment through novel therapies
15 September 2021 | Opinion | By Hithaishi C Bhaksar
A discussion on how new cancer treatments like cell-and-gene therapy are changing the treatment landscape for patients and healthcare systems.

Can you discuss how treatment options for DLBCL have evolved over the years?
Diffuse large B-cell lymphoma (DLBCL) is the most common subtype of non-Hodgkin lymphoma. It is an aggressive and complex disease which has different cell origins, gene-expressions and morphology. Historically, people with DLBCL haven’t had many options when standard therapies didn’t work for them. However, recent developments in cell and gene therapies and a deeper molecular understanding of DLBCL have rapidly shifted the landscape of treatment.
Initial treatment of DLBCL typically consists of chemotherapy plus a monoclonal antibody, rituximab (R-CHOP), and is often curative. Roughly one-third of patients relapse after receiving this first-line treatment. The most common treatment for such patients is Salvage chemotherapy regimen (SCR) with or without hematopoietic stem cell transplantation (HSCT). Studies have shown that around 50% of these patients risk relapse within 3 years and only a limited proportion of these second line relapsed / refractory (r/r) DLBCL patients are eligible for further treatment with allogeneic HSCT (allo-HSCT) - a treatment associated with a high rate of non-relapse mortality. For DLBCL patients relapsing after HSCT, median overall survival (OS) is as low as 4.4 months.
Unsatisfied outcomes for r/r patients have prompted efforts to discover new treatment approaches for DLBCL. We are seeing more individualised treatment for DLBCL according to novel genetic and molecular classifications.
In particular, cell and gene therapies have ushered in a new approach to the treatment of DLBCL and other life-threatening diseases. These therapies aim to treat, prevent, or potentially cure diseases by targeting the root cause of the disease at a genetic level, instead of just managing symptoms. This reduces or even eliminates the need for continuous, often life-long treatments.
Chimeric antigen receptor T cells (CAR-T) is a cell and gene therapy which has received FDA approval for the treatment of r/r DLBCL patients.
Can you discuss how CAR-T Therapy works and why it represents a new paradigm in the treatment of DLBCL?
CAR-T Therapy is a significant advancement in immune-based strategies and an embodiment of personalised medicine. More importantly, this treatment option offers new hope to patients who otherwise have had very limited options. CAR-T Therapy has also shown promising remission and survival rates in both clinical trials and real-world practice.
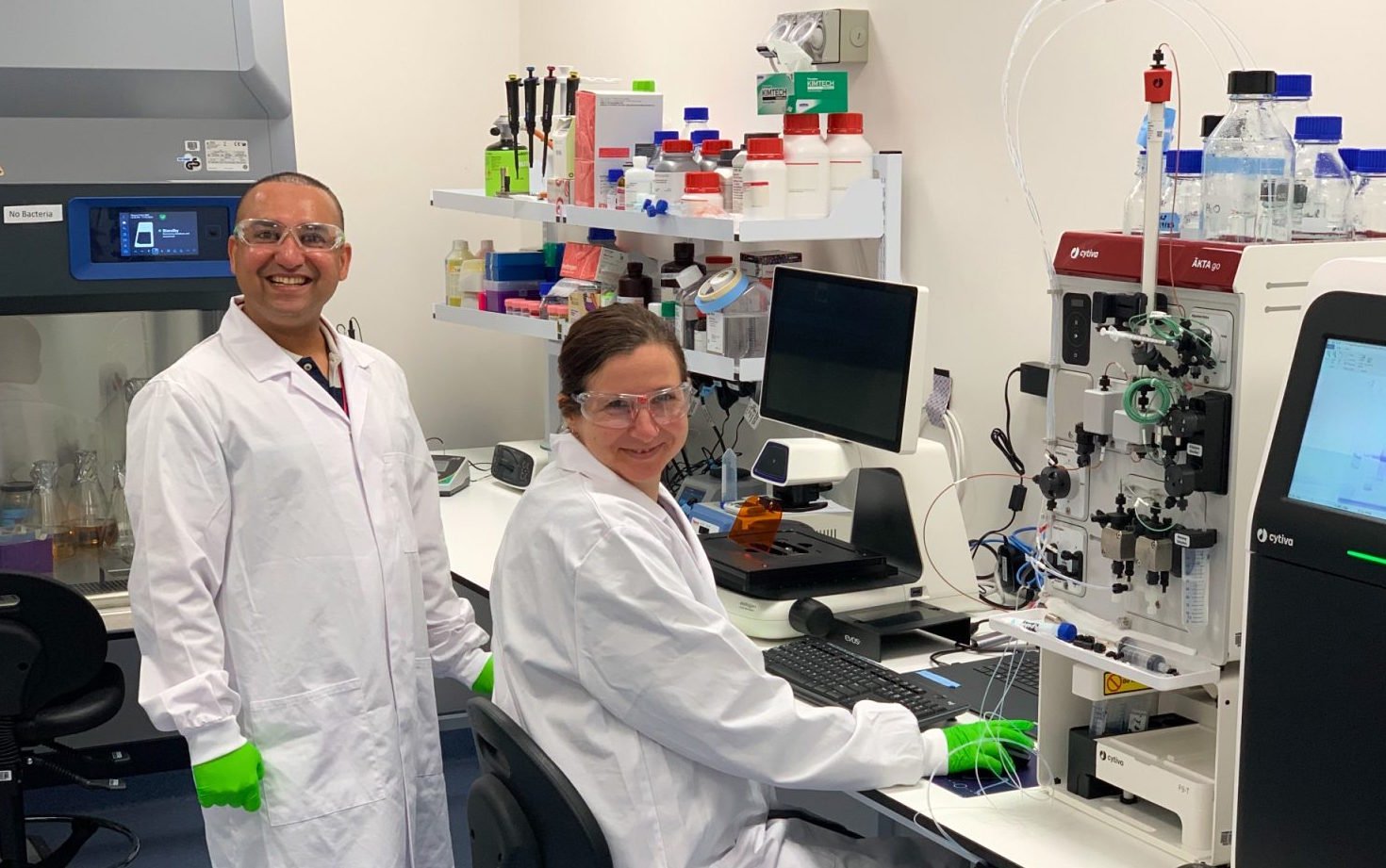
CAR-T Therapy uses a patient’s own immune system to fight certain types of cancers. This kind of therapy is a one-time treatment manufactured for each individual patient. The therapy first requires drawing blood from the patient via apheresis and separating out the T-cells. The T-cells are then cryopreserved and transported to a manufacturing facility.
Next, using a disarmed virus, the patient’s T-cells are genetically engineered to produce receptors on their surface called chimeric antigen receptors (CARs). These special receptors allow the T-cells to recognise and attach to a specific protein or antigen found on cancerous B-cells and other B-cells expressing a specific antigen. The CAR T-cells then undergo expansion in the laboratory. The resulting therapy is transported from the manufacturing facility back to the treatment centre and administered to the patient via infusion in one single session. The infused CAR T-cells recognise and kill cancer cells that harbour the antigen on their surfaces, and act as a living drug by further multiplying in the patient's body to destroy the future appearance of cancerous B-cells.
To date, CAR-T treatment can only be administered by designated qualified medical institutions with specific medical facilities and clinical care expertise. In March 2021, HSA approved the first CAR-T Therapy in Singapore, making Singapore the first country in Southeast Asia to offer the therapy commercially. Singapore General Hospital is currently the only hospital in the region to offer CAR-T therapy outside clinical trials.
What does CAR-T Therapy mean to the future of cancer treatment? Can the therapy be extended to other forms of cancer?
Cancer cells are known to hide from the normal immune system, but through CAR T-cell therapy, scientists are able to make T-cells better equipped to find and kill some cancer cells. CAR-T cell therapies have demonstrated remarkable efficacy for the treatment of haematological malignancies. The types of cancer that are currently treated using CAR T-cell therapy are diffuse large B-cell lymphoma (DLBCL), follicular lymphoma, mantle cell lymphoma, multiple myeloma, and B-cell acute lymphoblastic leukaemia (ALL) in paediatric and young adult patients up to age 25.
However, in patients with solid tumours, objective responses to CAR-T cell therapy remain sporadic and transient. CAR-T cells may be less effective against solid tumours because the cells and molecules surrounding tumours are often immunosuppressive, activating an immune checkpoint that causes the CAR-T cells to lose their activity. Fortunately, there are ongoing new research that looks into strategies to prevent tumour escape to CAR-T cell therapy. Scientists are finding new ways to target molecules of CAR constructs even more broadly to malignant solid tumours.
CAR-T has been one of the most significant recent advances in immunotherapies targeted at cancer. As research around CAR T-cell therapy continues, many in the cancer community can be hopeful around the therapy’s future and what it could mean for people with cancer.
Hithaishi C Bhaskar
hithaishi.cb@mmactiv.com