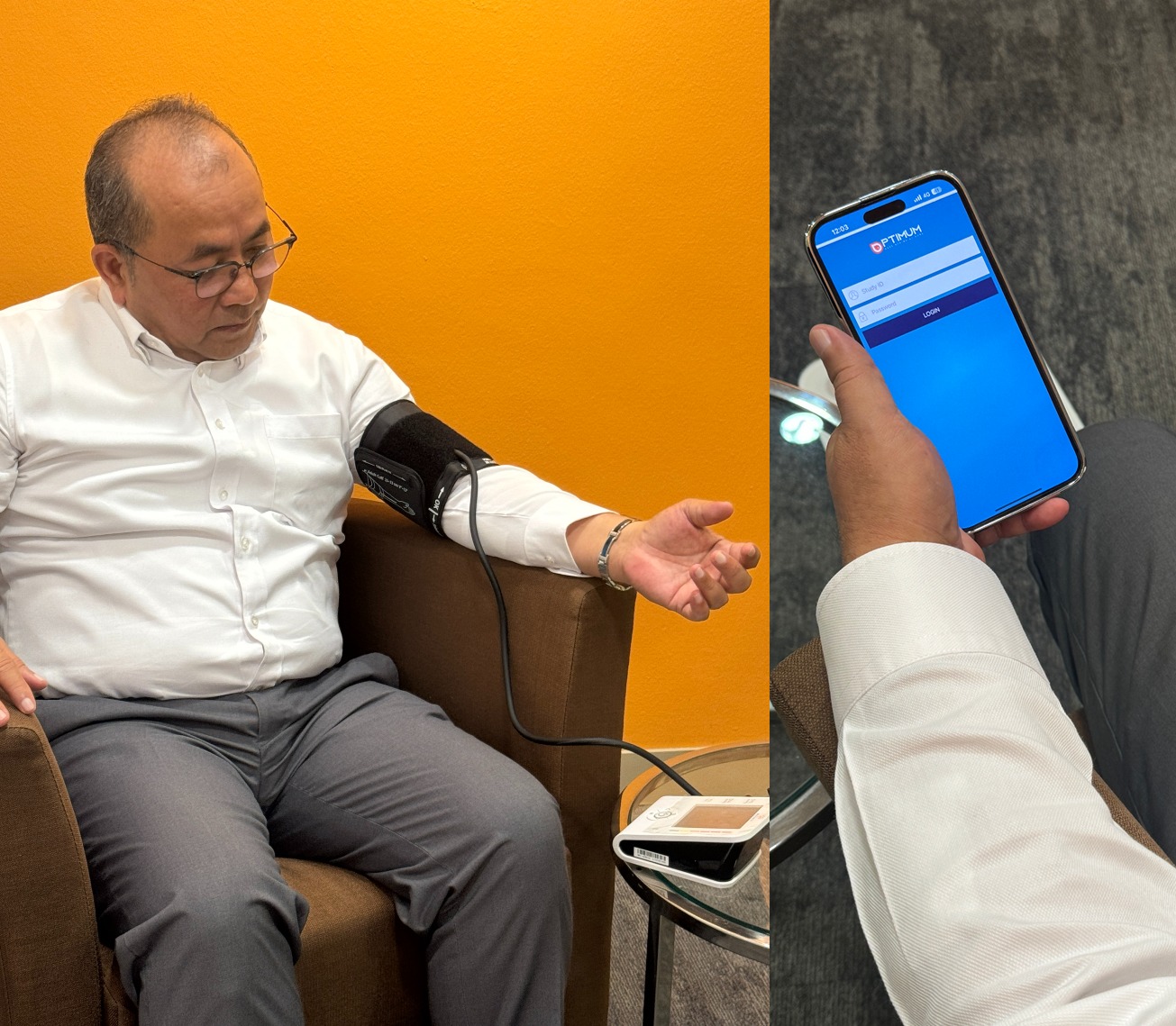
Image Credit: SingHealth Polyclinics (SHP)
Singapore’s SingHealth Polyclinics (SHP) in collaboration with the MOH Office for Healthcare Transformation (MOHT), has created a novel tele-monitoring system, known as OPTIMUM (Optimising care of Patients via Telemedicine In Monitoring and Augmenting their control of Diabetes Mellitus) for efficient and streamlined diabetes management.
The new system has demonstrated significant improvements in glucose levels, blood pressure, and cholesterol management among 160 patients with Type 2 Diabetes Mellitus (T2DM) over a six-month period. The clinical study was conducted at SHP-Sengkang from January 2020 to July 2023 with 330 eligible patients.
The study sought to evaluate the clinical outcomes of patients aged between 26 to 65 and were all diagnosed with T2DM with a recent HbA1c level of between 7.5 to 10%. The subjects were treated using OPTIMUM, in comparison to traditional standard care practices. In addition, it focused on a thorough comparison of several key health indicators in patients, including blood pressure, weight management, quality of life, medication adherence, confidence in self-management, diabetic literacy, and diabetes-related distress. In the intervention group, each patient received a comprehensive set of three Bluetooth- enabled devices designed for personal use throughout the randomised controlled trial (RCT) – a weighing scale, a glucometer, and an electronic blood pressure monitor. These devices were seamlessly synchronised with the OPTIMUM app on their personal smartphones.
Patients were guided through a structured programme over six months that included tele- education, where patients received weekly push notifications via the OPTIMUM app, encouraging them to engage in self-monitoring and educating them on diet and excerise educational videos designed to enhance patients’ self-management skills for T2DM. A brief quiz would be administered through the app after each video viewing to assess patients' comprehension. The six-month trial also required patients to monitor their body weight, blood pressure, heart rate, and capillary glucose levels. OPTIMUM's clinician dashboard was used by the study team for reviewing critical data.
The findings revealed a notable reduction in average HbA1c levels among participants in both the intervention and control groups over a six-month period. However, statistical analysis showed that the intervention group experienced a significant reduction of 0.34% in HbA1c levels compared to the control group.
In addition, reductions were observed in key health indicators, including weight, Body Mass Index (BMI), blood pressure (both systolic and diastolic), triglycerides, and fasting blood sugar levels in both groups. The patients in the intervention group showed statistically significant improvements in several areas, specifically in (a) Blood pressure, where the average systolic blood pressure (SBP) in the intervention group was 130.12 mmHg, which was lower than the control group’s average of 133.10 mmHg. (b) Total Cholesterol, where the intervention group had an average total cholesterol level of 4.18 mmol/L, which was lower than the usual care group’s average of 4.35 mmol/L. (c) Medication Adherence, where patients in the intervention group were five times more likely to take their medications as prescribed than the control group.
“The system was developed with input from both healthcare providers and patients, ensuring it meets real-world needs. A proactive tele-management algorithm based on established clinical practice guidelines and educational resources aimed at improving diabetes literacy are also key features. "By empowering patients and improving their management of diabetes, this advancement will lead to better health outcomes for Singaporeans with T2DM," said Dr Lee Cia Sin, Family Physician (Consultant), SHP-Sengkang. Dr Lee was one of the key research investigators on-site for this research study.
“Compared to participants who received usual care, those who participated in home tele-monitoring had significantly better health outcomes. Remarkably, these benefits continued even after the tele-monitoring phase ended, which demonstrates sustained improvements in health and medication adherence over the following 18 months,” said Clinical Associate Professor (Dr) Tan Ngiap Chuan, Director of Research and Primary Care Research Institute (PCRI), SHP and Vice-chair, Research, SingHealth-Duke NUS Family Medicine Academic Clinical Programme (FM ACP).




