For over a year the world has been battling the newly emerged infectious disease: the SARS-CoV-2 virus that caused the COVID-19 disease. With over 4.1 million deaths globally (as of July 27, 2021), the COVID-19 pandemic wreaked havoc within communities and triggered significant disruptions to the way we live, work, and socialise.
Across the Asia Pacific region, many countries continue to resist the impact of the pandemic and look to protect their citizens. India now has the second highest number of COVID-19 cases in the world - reporting over 400,000 daily cases at its peak for several days in May 2021. Several other countries in the region have seen the re-emergence of COVID-19 clusters, with particular concern around newly emerging COVID-19 variants across the world. Singapore also recently saw the emergence of new clusters and subsequent increase in cases, prompting the government to reimpose stricter guidelines on social gatherings to help prevent further spread of transmission.
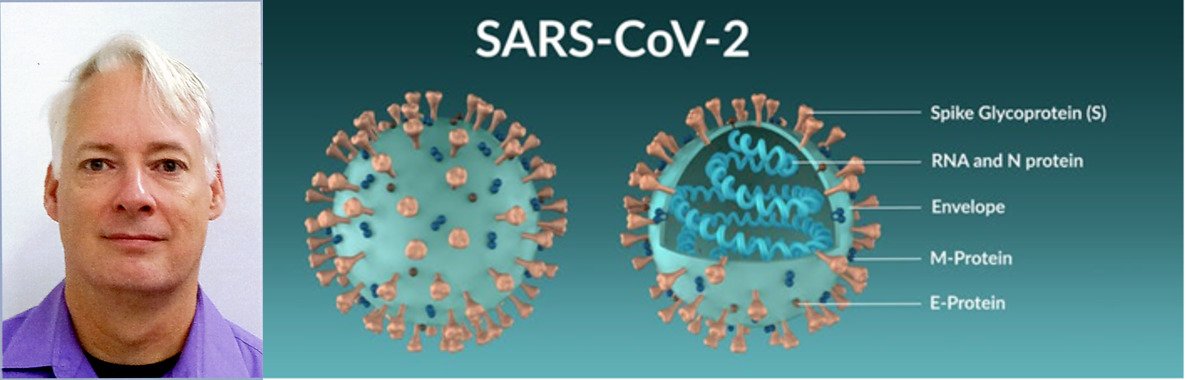
As the world continues resisting and adapting to the COVID-19 pandemic, academics and research scientists are looking to provide solutions to some of the unanswered questions about the causal SARS-CoV-2 virus. There are multiple research areas to investigate: the genetic make-up of the virus, its molecular structure, and the development of targeted therapeutics and preventative medicines – e.g., vaccines – to help eradicate the virus. In particular, one key focus within the research community has been the so-called “spike protein”.
Understanding the spike protein
Unlike many bacterial or fungal pathogens, viruses require a host cell to survive within the infected body. As indicated by the name, the spike protein sits on the outside of the virus and looks similar to miniature ‘spikes’. It is this protein that enables the virus to dock and then enter the host cell membrane, leading to the subsequent infection via viral replication.
In addition to enabling the virus to dock to the host’s cells, the spike protein is covered in complex glycan sugars, which help disguise the virus from the host’s immune system. If the immune system cannot recognise the spike protein as being a foreign object in the body, then the spike protein can interfere with the host cells without the immune system being able to stop it. Scientists believe it is this that makes COVID-19 such a deadly disease.
As the SARS-CoV-2 spike protein is crucial for the virus’ efficacy, large quantities are being harvested to enable researchers and commercial companies to develop antibody diagnostics, therapeutic antibody production, and also vaccine production.
The mRNA technology – used in the Moderna and Pfizer/BioNTech vaccines – specifically teaches the body to create its own spike protein replica, which the body recreates, its immune system identifies, and subsequently learns to target and destroy viruses with these particular spike protein make-up. Alternative COVID-19 vaccine technologies – such as adenovirus viral vector vaccines (e.g. Sputnik V) and recombinant protein vaccines (e.g. Novavax) – also demonstrate high efficacy against known variants. But with each new mutation and COVID-19 variant, there is a chance that the spike protein will also change, reducing the efficacy of the vaccine or even making the virus variant resistant to it. This makes continuous research into the virus’ spike protein a key element to combating the global pandemic.
Analytical instrument manufacturers like Agilent support researchers and commercial companies with their investigations into the SARS-CoV-2 virus and COVID-19, by providing a complete breadth of systems, consumables, software, services, as well as the knowledge needed to help customers achieve their research objectives.
Preventing the next pandemic
When looking to fight the spread of infectious diseases, it is also vital to consider how to prevent their emergence in the first place, or at the very least curtail transmission rates. A considerable number of infectious diseases originate within the animal kingdom, where they are normally limited to the spread within a single species. However, with the growing interaction between animals – both wild and domesticated – and humans, there is an increased risk that infectious diseases may transfect into humans, where they begin mutating and potentially causing more significant health complications.
These so-called zoonotic pathogens, which refers to the transmission of germs between vertebrate animals and humans, are relatively common across the world. Unbeknown to many, scientists estimate that ‘3 out of every 4 new or emerging infectious diseases in people come from animals’ according to the Centers for Disease Control and Prevention (CDC).
Some common diseases transmitted from animals to humans include malaria and dengue (which are from infected mosquitos) and Lyme disease (transmitted by tick bites). In Western Africa, the emergence of Ebola Virus Disease (EVD) in humans was first discovered in 1976 and to date, outbreaks still pose a threat since the most recent case was declared over on May 3, 2021 by the World Health Organization (WHO). Scientists hypothesise that people are initially infected with the Ebola virus through contact with an infected animal, such as a fruit bat or nonhuman primate. It is estimated that zoonoses are ‘responsible for 2.5 billion cases of human illness, and 2.7 million human deaths worldwide each year’. With the growing impact and potential harm that these pathogens could cause for humans, it is imperative that the global community comes together to tackle this issue.
This could take a two-pronged approach. Firstly, it is important that the natural habitat of wild animals is protected and not further enshrined upon. Veterinarian and disease ecologist, Dr Jonathan Epstein, commented, “The number one reason that pandemics happen is because of us, human activities, things that we do to the environment around us, whether it’s deforestation, agricultural expansion, land conversion, travel and trade. If we avoid damaging these ecosystems, it will actually protect human health by reducing the risk that a virus will emerge from those forests.” Secondly, it could be beneficial to develop and maintain a global set of hygiene standards for the global food industry, avoiding infectious disease contamination. The WHO estimated the global burden of foodborne diseases in 2015, which showed that “almost 1 in 10 people fall ill every year from eating contaminated food and 420,000 die as a result."
The marriage of research with prevention
Key learning from the COVID-19 pandemic is the recognition of the need for companies and governments globally to invest strategically into research laboratories that perform vital work towards greater understanding of these emerging viruses, as well as discovering new treatment options, including vaccinations.
The investment in research, however, needs to go hand-in-hand with reducing the possibility for zoonotic pathogens to easily transfer from the animal kingdom into the human world. Governments may consider enacting laws and internationally coordinated guidelines that would work towards preventing further infringement of the natural habitat of wild animals, as well as ensuring that the highest hygiene standards in the global food industry are maintained. By marrying research together with these preventive steps, we will all be far better prepared for the potential of a future pandemic.
Stephan Baumann, Infectious Disease Segment Manager, Agilent Technologies, USA




