Diabetic wounds often lead to severe complications that can result in amputations. These chronic and non-healing wounds are marked by persistent inflammation, affecting more than six per cent of the global population. In Singapore, there are about four lower limb amputations daily due to non-healing diabetic wounds. A study focusing on diabetic wounds in Singapore estimated that the gross amputation-related healthcare cost per patient was S$23,000 in 2017.
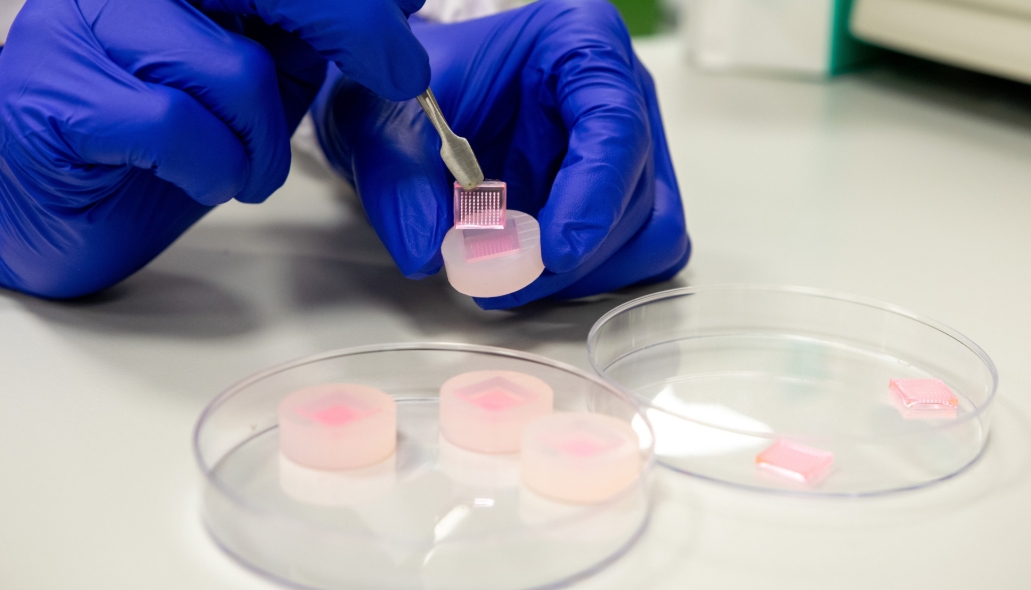
To address this challenge of great national and global importance, researchers from the National University of Singapore (NUS) have developed two microneedle technologies that have shown efficacy in accelerating diabetic wound healing in preclinical models by preserving the functions of proteins called growth factors, and removing undesirable inflammatory compounds.
In the first approach developed by the NUS research team, instead of delivering the growth factors directly, they first increased the production of growth factors within the wound. They achieved this by developing sucralfate microneedles (SUC-MN) to deliver an important immunomodulatory protein, interleukin-4 (IL-4), to stimulate the production of growth factors in diabetic tissues.
The research team screened different materials and eventually used heparin-coated porous microneedles (HPMN) to address the issue of persistent inflammation in skin wounds at the source.
The development of SUC-MN and HPMN represents a significant step forward in the field of wound healing and skin disease management. The team intends to conduct further studies to explore the potential of this technology and bring it to market.




