Novel platform can significantly reduces drug testing and screening time in cancer diagnosis
March 4, 2024 | Monday | News
Singapore's NUS and NCCS researchers have developed tissue-like bioengineered hydrogels, patient tumours can be preserved for up to 10 days, facilitating personalised screening of cancer drugs to enhance treatment effectiveness
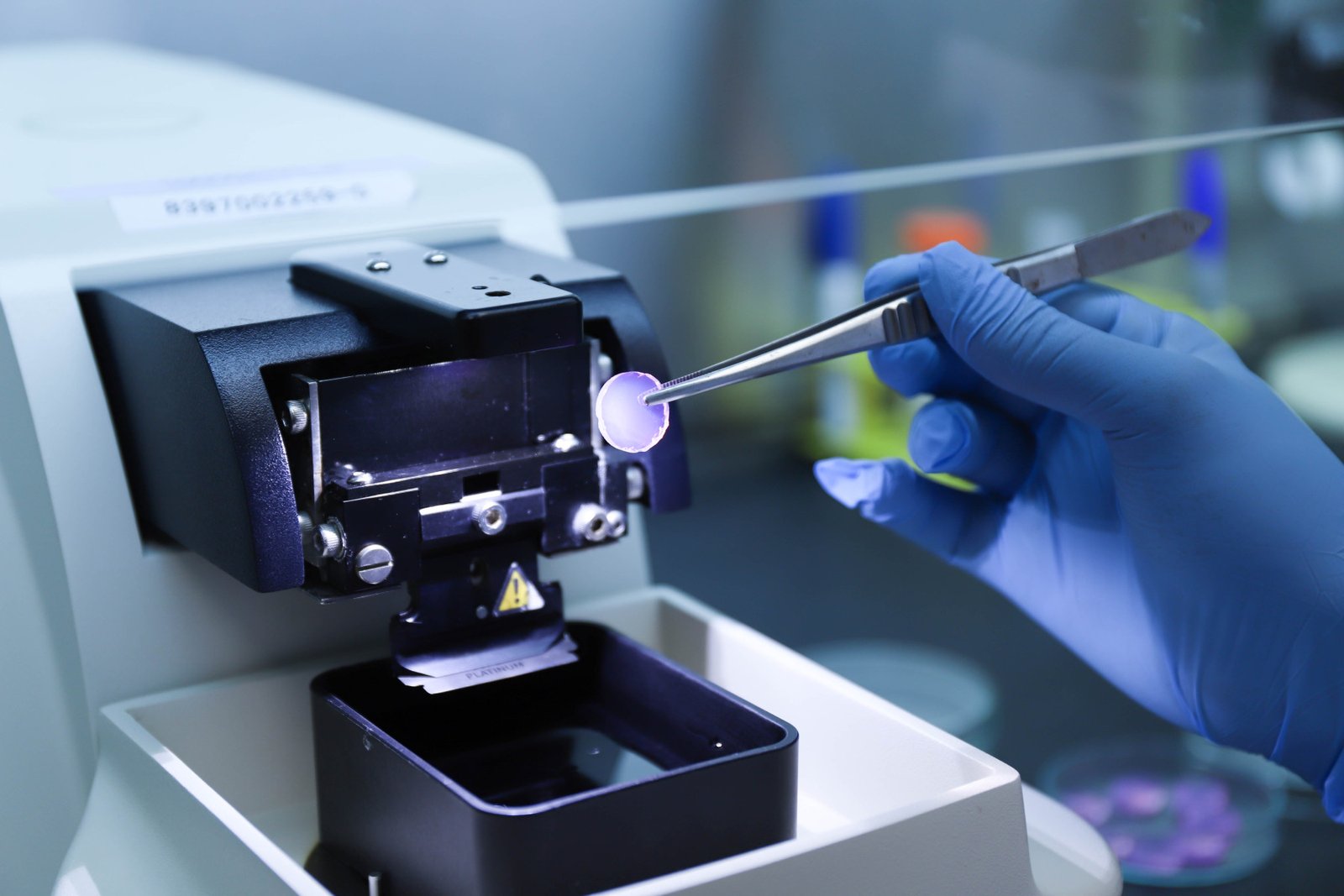
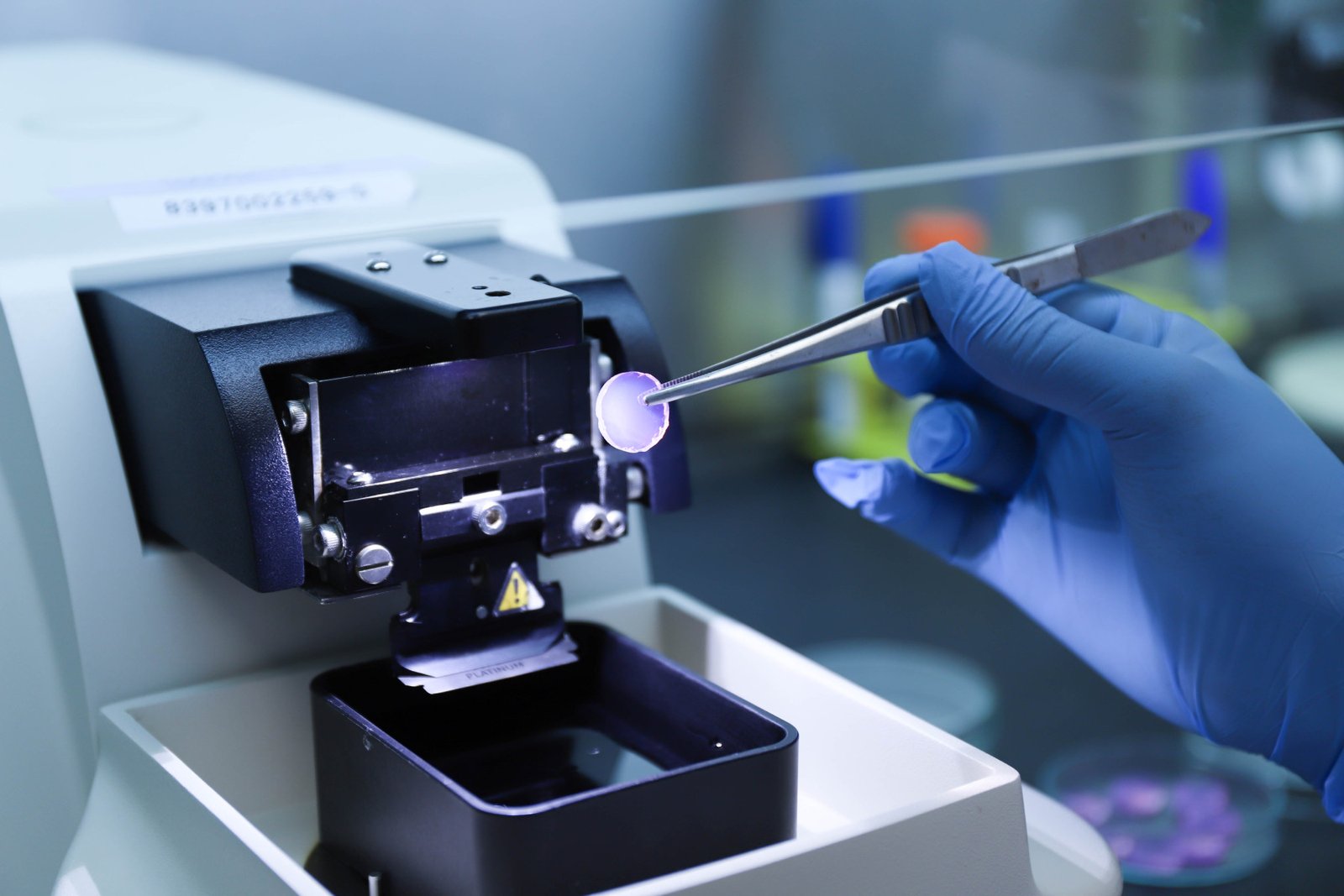
Photo Credit: NUS
In a breakthrough for personalised oncology, scientists from the National University of Singapore (NUS) and the National Cancer Centre Singapore (NCCS), have developed and demonstrated a novel platform that can significantly reduce the time needed to determine the efficacy of anti-cancer drugs.
In this first-of-its-kind technology, patient tumours resected from surgery can now be grown and better preserved ex vivo (outside of the body) compared to standard approaches, potentially accelerating the process for drug screening and testing for individual cancer patients. The breakthrough research use tissue-like, bioengineered hydrogels to keep the patient’s tumour alive even after it has been removed from the body.
A novel hydrogel-based platform to preserve patient-derived tumour slices
The study revealed several key findings. First, tumour fragments cultured in the platform were better preserved in terms of viability and morphology as compared to standard methods over time. The ability to maintain tumour fragments alive for up to 10 days allows for more drug testing and screening to be performed.
Second, through advanced characterisation including sequencing at the single-cell level, the researchers robustly demonstrated that all of the various chess pieces in the original tumour – including cancer cells, immune cells and fibroblasts – were also present in the cultured tumour fragments. The retention of the various pieces in the cultured tumour allows these ‘patient avatars’ to better depict the effects of drugs on cancer cells.
Furthermore, the study also showed the utility of these ‘patient avatars’ for testing immune checkpoint inhibitors, a type of immunotherapy, in a co-clinical trial. These ‘patient avatars’ could accurately predict the drug response of head and neck cancer patients from which the tumours were resected and cultured. Hence, the platform may help to guide clinicians in selecting patients to prescribe these immune checkpoint inhibitors, while reducing the possibility of giving the drug to patients whose tumours are least likely to respond to treatment.
Advantages of the new hydrogel-based platform
The use of this platform in cancer research has several advantages over traditional cell culture models. By preserving the tumour microenvironment, and maintaining the heterogeneity of the cells within the patient’s tumour, it offers a more accurate representation of the complex interactions between the different cell types in the tumour. This breakthrough allows researchers to study the effects of drugs and therapies in a more realistic setting, potentially leading to more effective treatment strategies.
Professor Gopal Iyer, co-lead of this study, who is a Clinician Scientist and Head of the Department of Head and Neck Surgery at the National Cancer Centre Singapore, said, “This platform allows us to test drugs in a more realistic setting with the goal of improving their efficacy. With this, we hope to alleviate some of the uncertainty and anxiety that can be a part of a patient’s experience when they undergo cancer treatment.”
The team is working on a larger-scale clinical trial to validate this new tissue-like, bioengineered material. They also hope to build a local repository of tumours for Singapore and the region that can be used for more comprehensive drug testing and pre-screening.