image courtesy: medium
Combination therapy with the PD-L1 inhibitor atezolizumab and the VEGF inhibitor bevacizumab significantly improves overall survival and progression-free survival in patients with unresectable hepatocellular carcinoma (HCC) compared to standard of care, showed results from a phase 3 study to be reported at the ESMO Asia 2019 Congress.
“This is the first study in 11 years to show an improvement in survival with a new first-line treatment option compared to sorafenib, which has been the standard of care throughout this time,” said study first author Ann-Lii Cheng, Director of the National Taiwan University Cancer Center, Taipei, Taiwan. He added, “Atezolizumab plus bevacizumab has the potential to be a practice-changing treatment option in hepatocellular carcinoma.”
Unresectable HCC is currently a major challenge in countries with a high prevalence of this cancer. Most patients in countries without screening programmes present with unresectable or advanced HCC because of the late appearance of symptoms, resulting in a very high mortality rate (almost 80%).
“Despite many studies over the past 11 years, we have been unable to find any better treatment option. This has been very frustrating because sorafenib has a response rate of around 10% and is associated with severe side-effects,” he explained.
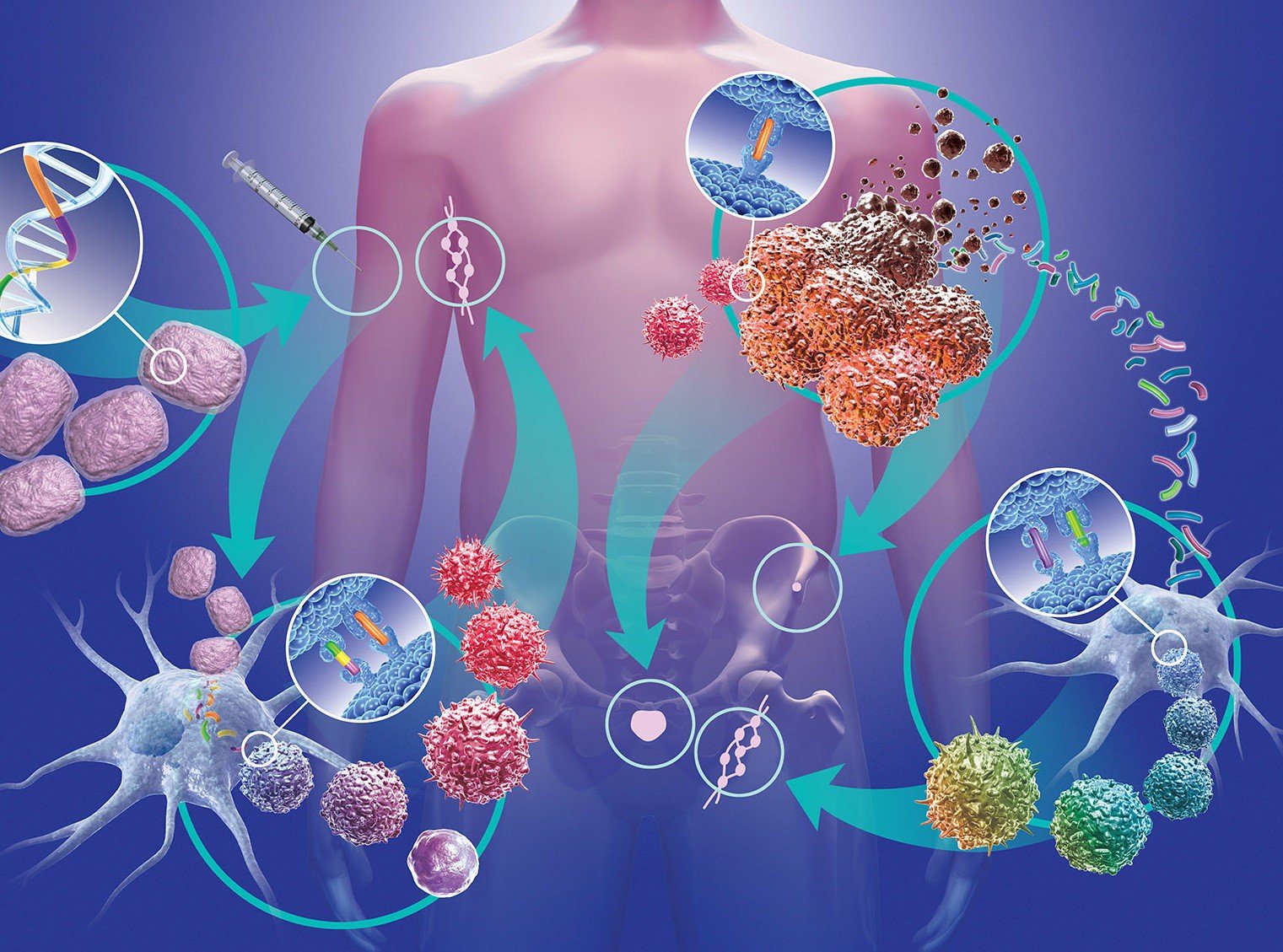
The phase 3 IMbrave150 study randomised patients with unresectable HCC to a combination of atezolizumab plus bevacizumab or sorafenib. Atezolizumab reactivates the immune response to tumour cells while bevacizumab stops tumours growing new blood vessels to obtain nutrients and oxygen but also helps upregulate host immunity to fight against cancer.
Results showed statistically and clinically meaningful improvement in the co-primary endpoints of overall survival and progression-free survival in patients treated with atezolizumab plus bevacizumab compared to those treated with sorafenib.
Commenting on the findings, Ian Chau, Consultant Medical Oncologist at the Royal Marsden Hospital, London, UK, said: “This is the first time a novel treatment has shown a survival benefit compared to the current standard of care. The results are very encouraging and there is a strong possibility this drug combination will be approved by regulatory authorities and be incorporated into international guidelines for advanced HCC.”
Angela Lamarca, Consultant Medical Oncologist at the Christie NHS Foundation Trust, Manchester, UK, agreed: “I think this is a breakthrough and based on the results, the combination of atezolizumab plus bevacizumab could become the new standard of care. The results are clinically meaningful in the setting of advanced HCC, as well as statistically significant.”
She considered the study was well-designed, with several strengths including its large sample size, with just over 500 patients, the use of a combination endpoint of PFS and OS, assessment of response/progression by a central reviewer and analysis based on the intention-to-treat population.
Lamarca also noted that the median follow-up of 8.6 months is relatively short, with the median OS for atezolizumab plus bevacizumab not yet reached. Chau agreed, noting that the improvement in OS is currently based on relatively immature data, with longer follow-up needed to confirm the magnitude of the OS benefit.
Looking to the future, Chau said, “The combination of atezolizumab plus bevacizumab will be very useful to patients with advanced HCC as a new systemic therapy but, with the high cost of immunotherapy and anti-angiogenic agents, it will also be important that those drugs are accessible to patients.”
Study results
The phase 3 IMbrave150 study randomised 501 patients with unresectable HCC on a 2:1 basis to atezolizumab (1200mg IV every three weeks) plus bevacizumab (15mg/kg IV every three weeks) or sorafenib (400mg twice daily). The overall response rate was more than twice as high with atezolizumab plus bevacizumab compared to sorafenib (27% vs 12%, p<0.0001). Atezolizumab plus bevacizumab delayed deterioration in the quality of life compared to sorafenib.




