The Chinese University of Hong Kong (CUHK) and The Hong Kong University of Science and Technology (HKUST) have unveiled ground-breaking research that sheds light on how COVID-19 infection may lead to late pregnancy complications.
The study reveals significant alterations in gene regulation within the placenta, paving the way for the development of potential molecular targets in future treatments to mitigate the detrimental effects of COVID-19 on maternal and fetal health.
Prior research involving 2,219 pregnant women with SARS-CoV-2 infection from various countries or regions, including Hong Kong, has demonstrated that SARS-CoV-2 infection increases the risk of pregnancy-related death, severe maternal morbidities, and adverse fetal and newborn outcomes.
Furthermore, a total of 142,561 cases of pregnant women with COVID-19 were reported in the United States between April 2020 and December 2022. The findings revealed that 11.21% of their infants born to these mothers were delivered preterm, and 9.7% required admission to the neonatal intensive care unit. Despite these findings, the underlying molecular mechanisms driving the increased risk of adverse pregnancy outcomes associated with COVID-19 remain to be fully understood.
The research team at HKUST, and CUHK identified dysregulation of angiogenesis genes at the maternal-fetal interface (MFI), potentially leading to abnormal blood vessel formation within the placenta and foetal growth restriction. Importantly, the observed molecular changes are likely due to the way the mother's body responded to the virus when she first got infected, rather than the virus directly affecting the MFI tissues in the placenta.
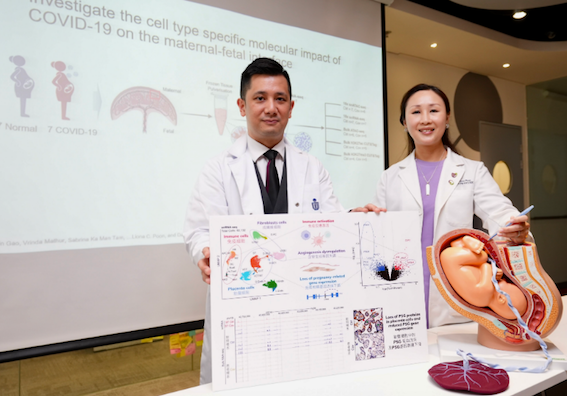
Professor Danny Leung, Associate Professor of the Division of Life Science and Director of the Center for Epigenomics Research at HKUST (left), and Professor Liona Poon, Chairperson of the Department of Obstetrics and Gynaecology at CU Medicine.




